Can Acid Reflux Affect My COPD?
Dear Dr. Mahler:
I have been having 2 - 3 flare-ups of my COPD in the past 6 months and am wondering whether my acid reflux could be causing these episodes. As background, I am 66 years old, have “moderate” COPD according to my PA, and am having heartburn most nights after dinner. I was told to take either an over-the-counter antacid or omeprazole, but neither of these have really helped much.
What do you recommend? Should I see a gastroenterologist about this?
Bruce from Taos, New Mexico
Source: COPD: Answers to Your Most Pressing Questions about Chronic Obstructive Pulmonary Disease. Mahler DA. Johns Hopkins University Press. Baltimore: 2022; page 40
Dear Bruce:
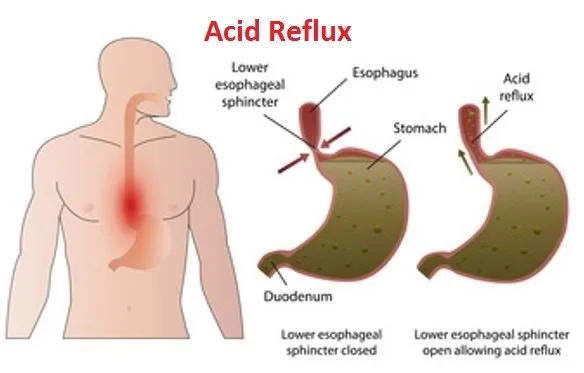
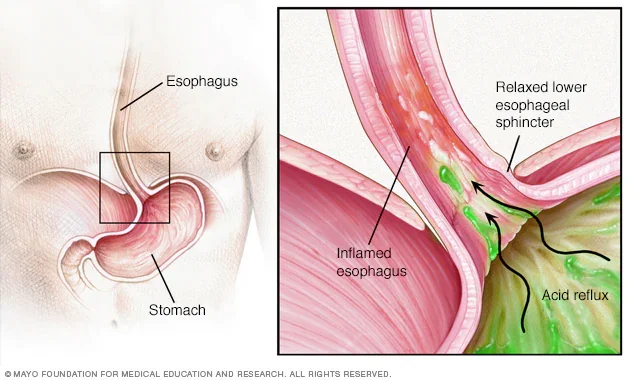
As you probably know, acid is normally produced when the food and liquids that you eat/drink enter the stomach. The acid helps to break down or digest the food/liguids before they enter into the small intestine. The term acid reflux refers to acid in the stomach moving up into the esophagus. Under normal circumstances, there is a sphincter (a ring of muscle that surronds the lower part of the esophagus) that opens to allow food and liquids to pass into the stomach and can close to prevent stomach contents from refluxing (moving up) into the esophagus (see Images). Acid reflux typically causes heartburn or indigestion - this medical condition is typically called GERD - gastroesophageal reflux disease. However, in some individuals, acid reflux may be silent and not cause any symptoms.
Detailed view of acid reflux
GERD is Common. It affects about 20% of adults in the United States. However, GERD is more common in those with COPD with estimates of 19% to 78%.
GERD is a risk factor for Flare-ups (exacerbations). In a meta-analysis of 13,245 patients with COPD, the presence of GERD was shown to significantly increase the risk of a flare-up with an average of about one-half additional exacerbtions per year (Huang C. BMC Pulmonary Medicine 2020).
How does GERD casue Flare-ups? There is some uncertainly as to the exact mechanisms. Howerver, the link between GERD and flare-ups is likely due to acid and/or liquids refluxing all the way up to the throat and then down into the lungs (called aspiration) and narrowing of the breathing tubes (bronchoconstriction) by nerve connections (i.e., vagal nerve) between the esophagus and airways.
Aspiration can lead to pneumonia and a flare-up which may be related to GERD or can be due to micro-aspiration of saliva, or bacteria carried on food and liquids into the lungs in combination with impaired immune function
Mangement of GERD may Reduce Flare-ups. Treatment recommendations require some changes in your life style. For example, if you are overweight, losing weight reduces the frequency of acid reflux. In addition, ideally you should not eat/drink anything for at least four hours before going to bed - this allows food and liguids in the stomach to empty and enter the small intestine. Certain foods/liquids - chocolate, caffeine, and alcohol - should be avoided at night as these relax the lower esophageal sphincter and make it easier for acid reflux to occur. Also, sleeping with your head and chest elevated using extra pillows or placing blocks under the head of the bed reduces reflux. Finally, there are over-the-counter as well as prescription medications (called protein pump inhibitors or PPIs) that work to reduce acid production in the stomach.
Bruce - in summary, I suggest that you try these recommendations:
Lose weight if you are overweight
Do not eat or drink for 4 hrs before going to sleep
Avoid caffeine, chocolate, and alcohol especially in the evening
Elevate the head of your bed (extra pillows, a wedge, and/or blocks under the legs at the head of the bed
discuss taking a prescription PPI medication (possibly at a higher dose
than you are using now) with your PA
If these do not help, then certainly you can discuss a referral to a gastroenterologist with your primary care professional.
Please note, the advice provided is not a substitute for asking your health care professional about your specific situation.
Sincerely,
Donald A. Mahler, M.D.